Skin problems in summer season:
1.Different types of skin problems and how to prevent them?
1. Sun burn:

Skin redness, swelling, and, in severe cases, cracking and shredding of the skin brought by excessive exposure on your skin.
Perhaps the most frequent summertime skin problem is sunburn.
Even if you use sunscreen and reapply it frequently,there’s a strong possibility that you’ve still experienced a painful red burn at some point.
To protect your skin, use sunscreen with an SPF of at least 30 every day.
Additionally, think about donning Unblocking clothing and a hat with a wide brim to protect your face.
If you do become sunburned, avoid the sun while it heals.
Skin damage may worsen with further sun exposure.
Sunburn is an inflammatory condition to UV radiation damage to the top layers of skin.
Melanin, the pigment that gives your skin colour and protects it from the sun’s rays, is at the root of it all.
Melanin works by browning exposed skin to the sun without protection.
Genetics control how much melanin you generate, which explains why some people burn from the sun while other tan.
Both are indicators of skin cellular deterioration.
People with less melanin may have sunburn, commonly known as red, puffy, and painful skin cells from prolonged contact to the sun without protection.
Sunburns can range in severity from minor to severe.
Your skin may start to peel if you get a sunburn.
Your body is attempting to get rid of this, as seen by this.
2.Heat rash:

A heat rash is a typical skin rash that can appear when you’re overheated or perspire a lot.
Due to the warming, certain areas of your skin may feel prickly or sting. Although it can itch a lot, it is not harmful.
A heat rash may be referred to as “prickly heat.”
Although anyone can develop a heat rash, newborns and young children are more likely to do so.
It is more likely to affect active persons, newborns in incubators, and individuals on bed rest who have a fever.
A bunch of tiny pimples or blisters on your skin brought on by sweat clogging your glands are known as a heat rash, prickly heat rash, or sweat rash. The rash could hurt or itch.
Keep your skin cold and dry at home to treat the rash.
If your rash persists for more than a week or cause suffering, call your doctor.
Sweat cannot leave your body when sweat glands become blocked.
It will accumulate beneath your skin and may cause a small, itchy rash of pimples.
The name “prickly heat” for this skin condition comes from the how the skin feels as the pimples explode.
By refraining from outdoor activities during the hottest portion of the day, you can assist avoid developing a heat rash.
Wear cool, loosening clothing as well. If you do sweat, be sure to wipe it off to keep your skin as dry as you can.
Consider having a chilly shower to help reduce your body temperature.
3. Folliculitis:

An infection called foliculitis develops in the hair follicles.
Although the lumps on folliculitis resemble pimples, they are frequently sensitive or uncomfortable.
Since sweaty skin encourages the growth of clogging bacteria, it is a frequent skin issue in the summer.
The easiest strategy to avoid folliculitis is to take a shower as soon as you can after perspiring. Avoid wearing sweaty clothes again.
Consider using a noncomedogenic sunscreen to your entire body to prevent accumulation in pores.
Hair follicles become irritated in the skin disorder known as folliculitis.
Usually, a bacterial or fungal infection is the culprit.
Around the microscopic pockets from which each hair grows, known as hair follicles, it may initially appear as small red lumps or white-headed pimples.
The infection may spread and manifest as crusty, non-healing sores.
Folliculitis is a skin disorder that develops when one or more hair follicles in a small area become inflamed.
It generally happens in irritated regions, such as shaving bumps, skin friction, or clothing rubbing.
Most often, folliculitis is caused by bacteria that ordinarily reside on the skin, particularly Staphylococcus organisms, infecting the inflamed follicles.
The following are some of the most frequent causes of folliculitis:
- Irritated skin after shaving.
- Rubbing from restrictive garment.
- An underlying dermatitis or skin disorders.
- Abrasions and other skin ailments.
- Prolonged exposure to plastic bandages or sticky tape.
4. Eczema flare-ups:

Eczema is a persistent illness that results with patches of irritated, flaming, and cracked skin.
Eczema flare-ups may be more prevalent in the summer.
Sweat can easily gather in the bends of the elbows and knees, which are locations where eczema frequently manifests, as hotter temperatures can irritate skin.
Strive to have a reasonable body temperature throughout the summer to lessen the chance of eczema flare-ups.
Keep your skin hydrated all season long, regularly rinse perspiration from your skin with clean water, and switch into new clothes frequently.
When skin is most irritated, a flare-up happens.
The following symptoms are present during the disease’s “active phase” or “acute phase”. Skin that itches a lot.
Additionally, it could hurt, and some people say they feel a burning sensation. A rash that looks flaky, dry, and red.
If it has been scratched, it may bleed slightly, be uneven, or swollen.Fluid that is moist or weeps when atopic eczema is particularly active.
Especially on the hands and feet, little water blisters might form.
Although acute eczema flareups can occur anywhere on the body, the face, scalp, chest, and hands are the most frequently affected areas.
Elbow, knee, wrist, and neck creases are among the joints that are frequently afflicted.
Eczema typically manifests as random flareups over the course of a person’s lifetime. Rashes might take several weeks to go away after treatment.
If you don’t restrict your exposure to triggers, there’s a chance that future flareups will happen as these rashes are the result of adverse immunological reactions.
5. Acne breakouts:

When your skin’s pores become blocked with bacteria and oil, acne develops.
Your body may perspire more when it’s hot outside.
Sweaty skin is more prone to gather oil and bacteria buildup, increasing the likelihood of acne breakouts.
Take extra steps to prevent sweating excessively if you have skin that is prone to acne.
Instead of rubbing sweat off your skin, gently pat it away to avoid aggravating your skin.
And never reuse dirty towels, caps, or apparel that has been exposed to perspiration.
When your hair follicles become clogged with oil and dead skin cells, acne is a skin disorder that develops.
It results in pimples, blackheads, or whiteheads.
Although it can afflict anyone at any age, acne is most prevalent in teenagers.
Although there are effective treatments for acne, the condition may continue.
The lumps and pimples heal slowly, and just as one starts to go, another one seems to appear.
A comedone is referred to as such if only the pore is clogged and there is no inflammation.
However, a comedone is referred to be a whitehead if it is closed (the pimple or zit looks whitish or yellowish).
A blackhead is a comedone that is open and has a black plug. The bacteria and oil in the pore, which turn black when exposed to air, are the source of this coloration.
Whiteheads and blackheads are not the same as pimples.
When a hair follicle becomes clogged with germs, it causes irritation and red pimples.
Acne affects people of all ethnicities and ages, but it is most prevalent in adolescents and young adults.
Males are more likely than females to get acne during the teenage years.
Acne can persist into adulthood, and when it occurs, women are more likely to experience it.
6. Ivy poison rash:

A plant known as poison ivy produces an oily substance that causes an itching skin rash.
Anyone who spends time biking, hiking, or enjoying the outdoors is likely to run across this issue.
Other frequent plants that can result in itchy, unpleasant rashes are poison sumac and poison oak.
Learn to recognise the leaves of sumac, oak, and poison ivy. You can avoid the leaves once you recognise them.
Wash your skin and clothes as quickly as you can if you come into touch with leaves.
Ointments containing hydrocortisone can relieve itching skin and speed up recovery.
In most climates, poison ivy develops as low shrubs or vines. A poison ivy plant contains three tiny leaflets on each of its leaves.
Within hours of exposure, touching any part of the poison ivy plant can result in red, swollen skin, blisters &itching.
Usually, a poison ivy rash goes away on its own in a few weeks.
Use an overcounter topical medication, such as calamine lotion, to calm sensitive skin in the interim. Cool compress and oatmeal baths may also be beneficial.
If you have a severe poison ivy rash or if it affects your face or genital region, consult your doctor.
A similar rash is brought induced by mango fruit rind, poison sumac, and poison oak.
You may go through the following stages of symptoms after being exposed to poison oak oil:
1. Itching skin:
You could initially feel an itching or stinging feeling at the location of exposure.
2. Rash:
A rash will start to develop as your reaction worsens. On light skin, this could seem red or pink.
The rash may seem purple, grey, black, or darker than the surrounding skin on those with black or brown skin tones.Patches of skin that came into direct touch with urushiol will experience this rash the hardest.
3. Blisters:
Your rash will start to develop blisters.These might enlarge and start to exude fluid. It is safe to drink this liquid.
4. Healing:
Your blisters will start to dry out as they ooze or pop. Once completely dried, they will gradually develop a crust and start to heal. It may take two or three weeks for this to happen and during that period you might still itch.
7. Bug bites:

In the summer, people spend more time outside, which exposes them to more bugs.
When female mosquitoes bite, a small amount of saliva is left on your skin, which triggers the histamine response in your body.
Your body is responding to the bite by producing the red, itchy bump.
Insects can’t get to your skin and attack if you’re wearing bug repellent and protective gear like long sleeves and pants.
However, if you do get bitten, avoid scratching the area.
Scratching an itching bite can aggravate your skin, cause more harm, and prolong the healing process.
A tiny, red lump on the skin that is frequently the result of an insect bite or sting can be uncomfortable and unpleasant.
Many bites can be safely treated at home and will disappear in a matter of hours or days.
If you were bitten or stung but did not see it happen, it may be challenging to determine what it was.
Being bitten by a bug can be unsettling, especially if you’re not sure what little critter caused the red, burning welt on your skin. Not to worry.
Common insect bites and stings are typically not harmful and recover rapidly.
However, some insect stings and bites, such as those from bees, hornets, fire ants, and wasps, can be extremely painful or even result in a life-threatening allergic reaction.
Others, such as bites from deadly spiders, necessitate rapid emergency medical attention.Bug bite symptoms offer hints as to the origin and intensity of the bites.
For instance, the majority of bug bites result in red lumps that hurt, itch, or burn. Blisters or welts can also develop after a bug bite. Here are some typical signs of an insect bite:
The only severe allergic reaction caused by bedbugs is a small, red, itchy bite mark on the skin.A red skin lump with white borders is the result of beestings.
Flea bites cause an itching welt to appear on the skin, typically on the legs and ankles.
In very rare instances, mosquito bites might cause severe allergic reaction or a swollen, painful pink skin lump.
Spider bites can result in relatively moderate symptoms like red skin, swelling, and localised discomfort, or more significant symptoms that require emergency attention.
Tick bites can cause a rash that resembles an enlarging bull’s-eye and ticks can transmit the disease Lyme.
Bedbug attacks frequently resemble other insect bites in appearance. Less about a quarterinch in diameter, the bites are extremely irritating. The bites frequently appear red on white skin. They can seem faintly pink or purplish on dark skin, and the longer they stay on the skin, the deeper brown they become.
The majority of insect bites result in red lumps that are uncomfortable, itchy, or burn. Blisters or welts could form on some bites.
Typically, a mosquito bite will be pink, raised, and itchy.
In contrast, a spider bite frequently results in red skin, swelling, and discomfort at the bite site.
Bedbug bites will be tiny and itchy, just like flea bites.
8. Athletes foot:

A typical sort of fungal infection that causes itchy, irritated skin between your toes is called athlete’s foot.
It can occur at any time of year, but it frequently gets worse if your feet are sweaty and you’re in a warm, humid atmosphere.
By keeping your feet dry and covered, you can prevent athlete’s foot.
In your shoes and between your toes, think about using an antifungal powder.
Don’t wear wet shoes and replace your socks if you sweat a lot through them.
A fungal skin illness called athlete’s foot typically starts between the toes. People who wear tightening shoes and have highly sweaty feet are more likely to experience it.
An itchy, scaly rash is one of athlete’s foot’s warning signs and symptoms. Contagious and spreadable by contaminated surfaces, linens, or clothing.
The tinea fungus grows on the feet and causes athlete’s foot. Direct contact with an infected individual or handling contaminated surfaces are both ways to contract the fungus. The fungus prefers warm, damp settings to flourish.
It is frequently discovered in showers, on the floors of locker rooms, and near swimming pools.
Everyone is affected by athlete’s foot. However, men and adults over 60 are the groups who are most frequently impacted. Diabetes may increase your risk of developing athletes foot obesity, a compromised immune system or and your feet may have injurious or tissue damage.
The bacteria and fungus on the foot’s surface that could lead to an infection can both be successfully eliminated by hydrogen peroxide.
Directly apply hydrogen peroxide to the afflicted region.
9. Melasma:

Patches of discoloured skin might form as a result of melasma. The face is the main area it affects, and patches are frequently brown or grey in hue.
Melasma is a surround condition for those who have it, however light exposure can darken spots.
The best approaches to manage melasma are to limit sun exposure and wear sunscreen, a hat, and protective clothing when you are outside.
A skin disorder called melasma is characterised by brown, blue-gray, or freckles like patches on the skin.
The cells that determine your skin’s colour produce too much of themselves, which results in melasma.
It is common, safe, and some treatments might be good.
Usually, melasma disappears after a few months.
Patches of skin that are darker than a person’s natural skin tone might emerge due to the skin disorder melasma,usually on the face.
Depending on the demographic, it might impact 1.5 to 33 percent of persons.
People with light brown complexion to darker skin tones are more likely to get melasma, especially in regions with extensive sun exposure.
Melasma, which can manifest as brown areas on the face, notably the cheeks, nasal bridge, and forehead, is more common in women.
The parts of the face where melasma most frequently manifests are:
- The nose’s nasal bridge.
- The cheekbones and the forehead.
- The top lip.
- The chin area.
Other parts of the body, particularly those that receive a lot of sunshine, may also develop melasma.
- the forearms.
- the neck.
- the shoulders.
Hyperpigmentation,or the emergence of discoloured area of skin or an uneven skin tone,is the main sign of it.
These areas are usually flat, appear darker than the person’s skin tone, and are frequently brown or grey in hue.
The look of these patches may irritate some people even when melasma has no apparent medical symptoms.
Melasma patches shouldn’t be physically painful.
Patches usually show up on the face.
The top lips, nose bridge, cheeks, and forehead are typical areas. There are also types of melasma:
1. Epidermal:
Epidermal melasma is characterised by a dark brown colour, a clearly defined border, and the ability to be seen under a black light. It can occasionally respond favourably to treatment.
2. Dermal:
Dermal melasma has a blurry border, light brown bluish colour, and does not change under a black light. It also does not respond well to treatment.
3. Mixed melasma:
The most prevalent of the three, mixed melasma has both bluish and brown patches, has a patterned under black light, and exhibits some therapeutic response.
Melasma is not unpleasant or harmful in terms of skin disorders, yet it can still be highly bothersome.
10. Skin cancer:

This summer, spending time in the sun may make you more likely to develop skin cancer.
The most prevalent form of cancer in the country is skin cancer, which is brought on by the sun’s dangerous UV radiation, which cause abnormal skin cell proliferation.
The best time to avoid skin cancer is between the hours of 10 a.m. and 4 p.m., when the sun is at its strongest.
Apply sunscreen to your skin and shield it from the sun by donning garments and a hat with a wide brim.
Skin cancer typically appears in sunexposed regions of the body, such as the scalp, face, lips, ears, neck, chest, arms, and hands in women, as well as the legs.
But it can also develop on parts of your body that are infrequently exposed to sunlight, such as your palms, the skin just below your finger or toenail, and your genital region.
All skin tones, including those with darker complexions, are susceptible to developing skin cancer.
People with dark skin tones are more prone to develop melanoma on the palms of their hands and soles of their feet, which are often not exposed to the sun.
1. Signs of the basal cell carcinoma:
Basal cell carcinoma typically develops on parts of your body that are exposed to the sun, including your face or neck. Basal cell cancer may manifest as:
A hump with pearls or wax.
A scar-like, that is brown or flesh-colored.
A wound that bleeds or scabs, then heals and reappears.
2.Signs of squamous cell carcinoma:
Squamous cell carcinoma most frequently affects your hands, face, ears, and other sunexposed regions.
On areas of the body that aren’t frequently exposed to the sun, those with darker skin are more likely to develop squamous cell carcinoma.
Symptoms of squamous cell carcinoma include:
A solid, rosy nodule.
A flat, crusty lesion with scaly edges.
3. Melanoma:

The cells that make melanin, the pigment that gives your skin its colour (melanocytes), which is the most dangerous type of skin cancer, are where melanoma begins.
Additionally, melanoma can develop in your eyes and, very rarely, inside your body, like in your throat or nose.
The actual reason why all melanomas occur is unknown, although being exposed to ultraviolet (UV) radiation from sunshine, tanning beds, or tanning lamps increases your risk of getting the disease.
You can lower your chance of developing melanoma by limiting your exposure to UV light.
2.Prevention of skin problems:
1. How to prevent sunburn?
The use of sunscreen and protective gear is one approach to avoid being sunburned.
Chemicals in sunscreens filter or block sunlight.
Lotions, creams, sprays, and powders are all forms of sunscreen.
Some, like oxybenzone and avobenzone, have compounds that filter and absorb sunlight.
Others have substances like zinc oxide or titanium dioxide that physically block the light.
No sunscreen completely blocks UV rays. However, they aid in skin protection.
1.Utilizing sunscreen:
Don’t forget to use sunscreen with an SPF of 30 or higher.
Select a sunscreen with a broad spectrum that blocks UVA and UVB rays.Use sunscreen that is waterresistant or waterproof.
Apply to all exposed skin, including the tops of the feet, ears, lips, and the back of the neck.30 minutes before leaving, apply it.
2. Other ways to avoid sunburn:
From 10 am to 4 pm, avoid being in the sun.
The UV rays of the sun are at their peak during this time.
Put on a hat with a broad brim.
Put on clothes that will shield your skin from the sun.
Some apparel has a UV protection factor rating (UPF).
Avoid using tanning beds.
Search for shade.
UV radiation is reduced in shaded locations.
even in areas of shade, use sunscreen.
It is simple to head outside for some sunfilled fun, but you must use sunscreen and take the necessary steps to avoid being sunburned and ruining your day.Sand, snow, cement, and water are a few more surfaces that reflect UV rays.
How to protect your skin from sun?
At least 15 to 30 minutes before going outside, apply at least one ounce of sunscreen (enough to fill a shot glass).
Make sure it has an SPF of 30 or more and is water-resistant.
Other sunscreens might aid in preventing sunburn, but they won’t offer skin cancer protection.
Use sunscreen again every two hours. In case you are swimming or perspiring, reapply every hour.
When near water or sand, exercise particular caution.
Spend as little time in the sun as possible between 10:00 AM and 4:00 PM.
The sun is at its strongest at this time.
Use the shadow rule to your advantage if your shadow is shorter than you, the sun’s rays are greatest and you should seek shelter.
Wear long pants and a long-sleeved shirt if you can.
More sunlight is blocked by dark garments with tightly woven fabric than by white or loosely woven clothing.
Look for clothing created with specific sunprotective fabric for added coverage.
Wear sunglasses and accessorise with a hat that covers your face, neck, and ears.
The eyes and surrounding skin are best protected with sunglasses with lenses that block 99 to 100 percent of UV rays.
2. How to prevent heat rash?
Keep your skin cold above all else to avoid perspiring and aggravating the rash.
Wear loose cotton clothing and lightweight bedding to keep your skin cool.Use chilly showers or baths.
Consume plenty of liquids to prevent dehydration.
Apply something cold, like a moist cloth or an ice pack (covered in a tea towel), for up to 20 minutes to soothe the irritating or prickly sensation.
Avoid using fragrant shower gels or creams and instead tap or pat the rash to prevent itching.
If the affected region is kept cold and dry, heat rash typically goes away on its own in a few days.
Therefore, keep your body cool by using a fan or an air conditioner. You can also take a cool bath or shower and let your skin air dry.
Avoid using any oilbased products after the skin has become cool and dry again since they could clog your sweat glands.
Call your doctor if your prickly heat does not subside within a few days or if you experience an infection where the bumps have ruptured.
If you have a fever or any other symptoms of disease, you should also call the doctor.
Avoid hot, humid settings and other situations that can cause excessive sweating to help prevent heat rash.
When it’s quite warm outside, stay away from vigorous exercise.
Wear light, loosefitting clothing and use air conditioning, fans, chilly showers and baths to keep cool when it’s sweltering outside. Stay away from synthetic textiles.
To keep hydrated and to help the body chill down, drink lots of liquids.
3. How to prevent Folliculitis?
The type and degree of your folliculitis, the skincare techniques you’ve already tried, and your preferences will all influence your treatment options.
Options include prescription drugs and surgical procedure like laser hair removal. The infection could return even with treatment.
Medication:
Tablets or creams to treat infections. Your doctor could advise using an antibiotic cream, lotion, or gel for minor infections.
It is uncommon to treat folliculitis with oral antibiotics.
However, your doctor could advise them if the infection is severe or keeps coming back.
Folliculitis can be avoided by keeping your skin clean, dry, and free from abrasions and irritations.
Infections are more likely to affect some patients than others, such as diabetics.
These precautions might be particularly critical if you suffer from a medical condition that increases your risk of contracting infections.
It is generally not advised to regularly use antiseptic washes because they can dry out and irritate the skin.
Moisturizing the skin can help shield it from harm.
Use caution when shaving (particularly if you wet shave), and moisturise the skin with shaving gel, foam, or soap to prevent nicks and cuts.
In many situations, altering your lifestyle behaviours can help you prevent or manage folliculitis.
Bacteria and yeast typically invade your hair follicles during folliculitis infections.
You can reduce the quantity of infectious material in your hair follicles by altering a few aspects of your typical self-care routine.
Here are a few pointers for avoiding it:
- Cleansing your skin.
- Shaving restrictions.
- Examining the hot tubs and heated pools’ chemical disinfection levels before utilising them.
- The faster the chemicals break down in a hot tub or pool, the less effective they are against bacteria.
- The faster the chemicals break down in a hot tub or pool, the less effective they are against bacteria.
- rinsing off and taking off your swimwear after using a hot tub or pool.
- Wearing breathable clothing prevents sweat from getting sucked into the spaces between your garments.
Folliculitis comes in a variety of forms. Most varieties are not easily spread from person to person and are not contagious.
Sharing towels, razors, or hot tubs can all result in the spread of infectious organisms that cause folliculitis.
If you’re not careful, it can potentially spread from one body part to another.
4. How to prevent Eczema flare-ups?
5 ways to prevent eczema flare-ups:
Do you occasionally have red, itchy patches on your skin?
If so, you might have eczema like the 30 million other Americans.
A group of skin disorders that cause rashes are collectively referred to as eczema, sometimes known as dermatitis.
Eczema in its most prevalent type is atopic dermatitis.
Your cheeks, elbows, knees, hands, or feet may develop eczema.
Although the redness and inflammation may seem concerning, they are not infectious.
Although the specific cause of eczema is unknown, you are more likely to have it if one of your parents does.
Flareups may also be influenced by certain environmental conditions.
1. Restrict your contact with specific home items:
Try to stay away from these things if you can identify what sets off your flare-ups.
Certain home things are more likely to start an episode of itchy eczema if you can’t identify your triggers.
Avoid or record your interactions with:
- Polyester and wool.
- Soaps with scents.
- Laundry soaps.
- After-shave creams.
- Turpentine and other cleaning agents.
- Specific home cleaners.
2. Wear gloves:
The act of remembering to put on gloves before venturing outside in the cold shouldn’t be challenging.
When it’s cold outside, wearing gloves not only keeps your hands warm but also shields them from the dry, itchy air that can aggravate eczema.
When doing dishes or other tasks that expose your hands to chemicals or other irritants, you should also wear gloves, preferably plastic ones.
You don’t want your hands to start perspiring, so make sure to occasionally remove the gloves from your hands.
Additionally, sweat can make your eczema worse.
3. Use proper shower and bath etiquette:
Short, warm showers or baths are recommended.
The dryness caused by taking long, hot showers can make your skin more prone to flare-ups.
Use a moderate amount of unscented bath products.
When you’re finished, pat yourself dry with a nice towel.
To assist your skin best absorb the moisture and seal it on apply moisturiser as soon as you get out of the shower, while it’s still damp.
4. Moisturise:
Dry skin is often irritated. It becomes tight and brittle, which might cause an eczema flare-up.
Applying moisturiser all over your body at least twice a day will help prevent dry skin. Select moisturisers free of fragrance and other unnecessary additives.
Thin, liquid moisturisers are preferable than creamy, thick ointments and lotions.
5. Reduce tension:
Scratching your eczema aggravates it, as does becoming anxious about it. Additionally, overall tension can cause a attack to flare up.
Finding ways to minimise stress in your life and using stress reduction like deep breathing and meditation can help prevent an eczema flare-up.
5. How to prevent acne breakouts?
You might be shocked to hear that routine daily activities could be exacerbating your acne.
Follow these straightforward suggestions to clear up your skin and say goodbye to breakouts:
1. Acquire some face washing skill properly:
You should wash your face every day as part of your skin care regimen to get rid of debris, sweat, and extra oil.
However, if you wash your face too frequently or with the incorrect cleanser, you might exacerbate your acne.
So, how should one cleanse their face properly?
Pick a mild, alcohol-free cleanser first.
Apply the acne cleanser to your face after wetting it with warm water and gently massaging it in a circular motion with your fingertips using clean hands or a clean washcloth. Rinse well, and then dry your face with a fresh towel.
Wash your face twice a day, once in the morning and once before bed, to keep it clear and pristine.
Instead of washing your face again if it feels oily during the day, use blotting paper to absorb the extra oil.
After working out, you can wash it again if you sweat a lot, but don’t wash it too frequently or you’ll dry out your skin and make things worse.
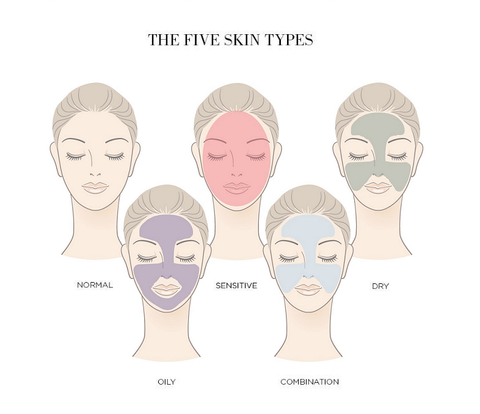
2. Choose right skin care products:
To maintain your skin supple and soft if it is dry, search for items that hydrate and strengthen the outer layer of defence.
Clay or charcoal masks, foamy cleansers, and skincare products with alcohol should all be avoided because they will just exacerbate your skin’s already existing dryness.
Choose moisturising moisturisers and gentle cream cleansers instead. You might also try using face oil at nighttime before sleeping.
For oily skin, you want to get rid of extra oil without entirely drying out your skin.
Avoid using face oils and thick, oilbased lotions, as well as abrasive scrubs that could remove too much oil.
To help prevent breakouts, choose waterbased, oilfree serums, thin gel moisturisers, and salicylic acidcontaining products.
Depending on the type of skin you have in each location, you may need to apply different products on your cheekbones and jaw than you do on your Tzone if you have combination skin.
Stay away from thick moisturisers, foamy cleansers, and clay masks.
Stick to mild lotions and gentle cleansers instead, applying stronger moisturisers as necessary to dry areas.
3. Utilize makeup suit for acne:
You might be tempted to disguise a fresh pimple on your face with cosmetics, but that is actually one of the worst things you can do.
Too much or the wrong kind of cosmetics can clog your pores, causing outbreaks.
Not that you shouldn’t wear cosmetics; just be cautious about the items you pick and the methods you employ.
Try a tinted moisturiser or choose a thin layer of powder foundation in place of thick makeup.
To obtain the desired result, stay away from greasy formulas and try to wear as little makeup as you can.
Look for noncomedogenic (which basically means that the product is engineered not to clog pores) and fragrance & chemicals cosmetics when purchasing makeup.
4. Drink water:
You could believe that your skin is overhydrated if you have oily skin, yet the contrary may be true.
In actuality, if you are not drinking enough water, you might still have oily skin and be dehydrated.
Your skin’s protective barrier is damaged when it is dehydrated, which causes irritation.
The hormones that stimulate sebum production are then brought on by that irritation, resulting in clogged pores and more frequent breakouts.
Drinking water throughout the day will help maintain your skin moisturised and healthy as it is composed of more than 60% water.
Although the CDC does not have a daily recommendation, it is widely accepted that 8 to 8 oz of water should be consumed daily.
5. Keep your skin moisturized:
Water, fat, and other materials make up the protective layer that is your skin.
The sebaceous glands create more oil when the skin itself becomes drier, which accumulates on the surface and clogs your pores.
To keep your face naturally hydrated and acnefree, the finest moisturiser contains water and oil.
Pick a moisturiser that is appropriate for your skin type to start. Next, check to see if it contains any drying agents, such as alcohol.
Hyaluronic acid and glycerine moisturisers help to lock in moisture and keep your skin supple all day.
Before applying a moisturiser, wash your face with warm water for the best hydration. Pat your skin dry so that it can absorb some of the water.
Use a tiny quantity of moisturiser when you are ready to apply it, and massage it into your skin gently without rubbing it in too much.
6. Do not touch your face:
Even if you wash your hands frequently, there are still numerous germs and bacteria living on your fingers that could be spread to your skin if you touch your face.
You might be introducing dirt and other pollutants to your skin every time you touch your face, which might clog your pores and result in a breakout.
Avoid touching your face when you are experiencing an active breakout.
While popping or squeezing pimples may feel good in the moment, you could end up causing more inflammation and worsening the condition.
The pitting and scarring that can result from popping pimples may eventually become permanent.
7. Try medications:
The best prescription treatments for acne are listed below for your consideration:
1. Tretinoin:
Tretinoin, a kind of retinoid, has comedolytic effects that aid to clear pores, promote cell development, & regulate sebum production.
2. Benzoic acid:
Azelaic acid, which is frequently used at a 20 percent concentration, has antiinflammatory properties and can be used to treat mild acne.
3. Peroxide of benzoyl:
Benzoyl peroxide, one of the most often used component in acne treatments and gels, aids in the destruction of acne-causing bacteria and the drying of active outbreaks.
It is available in concentrations of 2.5 percent, 5 percent, and 10 percent.
4. Acid salicylate:
Salicylic acid, which is similar to benzoyl peroxide in that it heals acne without overly drying or harming the skin, also possesses keratolytic qualities that aid in exfoliating the blemish.
8. Clean and protect your pillow case:
The dirt, sweat, hair products, and makeup from your face seep into your pillow because you spend up to onethird of your life sleeping, especially if you don’t wash your face before bed.
You’re not doing your skin any favours by sleeping on a dirty pillowcase because you’re sleeping in all of that debris.
You should wash or replace your pillowcase once a week in addition to cleaning your face every night before bed.
Make sure your pillowcase is clean and free of oil if you have oily skin and do it more frequently.
9. Protect your skin from sunlight:
If you’re going outside between the hours of 10 AM and 4 PM, it’s also a good idea to protect your skin by donning sunglasses and a wide-brimmed hat.
Take additional care if you’re using any of these prescriptions because they can have side effects that make your skin more sensitive to the sun, including antibiotics, antiinflammatories, and blood pressure medications.
Additionally, the acne treatment tretinoin may make your skin more sensitive to the sun, making it all the more crucial to use sunscreen in addition to tretinoin.
10. Use healthy diet:
Grains (glycemic), colourful fruits and vegetables, leafy greens, oily fish, nuts, seeds, beans, and legumes are the healthiest foods for your skin.
Foods with antiinflammatory characteristics can be helpful and antioxidants in particular are good for skin health.
You may significantly lessen the severity and frequency of acne breakouts by taking good care of your skin.
However, what if you already have one or two pimples?
Don’t touch it, first of all!
Even though popping a pimple could be appealing, doing so can actually push the pus and bacteria deeper into your skin, causing more inflammation and aggravating your blemish.
6. How to prevent poison ivy rash?
The Source advises thorough body washing with lots of lukewarm water and soap if you believe you have come into touch with poison oak.
You should take extra care when doing this to inspect your hands, fingernails, and any skin that may have come into touch with the plant.
The plant’s oils may linger on clothing and other items, which may cause you to develop new rashes.
Clothes and other items that may have come into contact with the plant should be washed.
The rash may itch, and you could feel the need to scratch.
Scratching blisters or rashes, however, can damage your skin’s protective barrier and result in an infection.
Take lukewarm water.
Cover up in locations where poison ivy is likely to thrive by donning protective garments.
When gardening or removing poison ivy, wear rubber or thick gardening gloves because thinner hands may allow the oil to get through.If exposure occurs, a person must remove these substances as quickly as feasible.
Everything that comes into contact with the plant should be thoroughly washed. Rub alcohol or soap and water can be used to thoroughly clean anything that has come into contact with poison ivy.
1. Get rid of ivy poison in the garden:
The best approach may be professional removal because merely coming into contact with the roots, a dead plant, or smoke from a burning plant might provoke an allergic reaction.
Poison ivy should never be burned because the smoke it produces might trigger severe allergic reactions.
2.Get a poison ivy kit ready:
Having a variety of poison ivy remedies on hand, including rubbing alcohol, water bottles, and soap, can enable quick treatment to lessen exposure, which can lessen the intensity of symptoms.
7. How to prevent bug bites?
Despite the fact that the majority of insect bites are harm, some can spread harmful conditions such the dengue virus, Lyme disease, and malaria.
It’s crucial to take precautions to lower your risk, if you’re travelling to regions where recognised insectborne diseases are prevalent.
Dermatologists suggest the following precautions to help avoid bug bites:
Apply repellant on the skin.
Use insect repellent that contains 20 to 30 percent exposed skin and clothing to protect against mosquitoes, ticks, and other pests.
Always read the label on the repellent and reapply as necessary.
Apply your sunscreen first, let it dry, and then apply the bug repellent if you’re also wearing sunscreen.
Avoid using sunscreen that also contains insect repellent because sunscreen needs to be applied frequently and liberally while repellent should only be applied seldom.
8. How to prevent Athlete’s foot?
A common fungal illness called “athlete’s foot” affects the skin on the foot, particularly in the space in between the toes.
It might also spread to other bodily parts if left untreated.
When the foot becomes sweaty and heated within the shoe, which creates the ideal environment for the fungus,the infection typically manifests around the spring or summer.
The burning, redness, flaking, and itching are the most typical symptoms. The foot’s skin can occasionally crack, which increases its susceptibility to bacteria.
We have put together a list of nine suggestions to help you avoid athlete’s foot this summer:
1. Steer clear of tight fitting shoes:
Your feet feel the squeeze of tight, bulky shoes.
Your feet get caught in a steamy atmosphere with little air to dry out the dampness, which increases their susceptible to developing a fungal infection.
2. Invest in quality shoes:
Shoes made primarily of plastic have a lower rating for ventilation and heat up more quickly than shoes made primarily of leather or canvas.
3. Avoid swimming pools & gyms:
Public swimming pools and gyms are examples of warm, humid places where the bacterium that causes athlete’s foot thrives. If your immune system is less robust.
4. Maintain dry feet:
The Trichophyton bacteria requires both heat & moisture to survive.
No matter how hot it is outside, if your feet remain dry, you won’t have fungus on your skin.
Talcum powders with antifungal properties are a cheap way to keep your skin dry and pleasant all day.
5. Take off your shoes after working out:
After your workout, take off your shoes and wash your feet with antibacterial soap to get rid of any remaining bacteria.
6. Avoid to lending out your shoes:
Sweat is a breeding ground for the fungus that causes athlete’s foot, and even a small amount of it can produce an infection, especially if your immune system is weak.
7. Put on socks made of organic material:
Even while cotton and silk socks are more expensive, they also breathe better.
They not only lessen your risk of developing athlete’s foot,but they also make your skin feel cooler and more pleasant in the summer.
8. Put sandals on:
Wear sandals if at all possible. You’ll be able to breathe freely and lessen the temperature of your skin as a result of the sweat being dried off.
9. Investigate ways to strengthen your immune system:
It’s not always possible to boost your immune system, particularly if you’ve just undergone chemotherapy or an organ transplant.
However, if you’re generally healthy but frequently get fungal infections, you might want to consider increasing your intake of antioxidants and vitamins.
10. Contact to a specialist to avoid complications:
To prevent complications, consult a specialist.
Athlete’s foot is simple to treat, but if it doesn’t go away after using antifungals, it may be time to see a doctor. A doctor can help you develop a personalised treatment plan and reduce the risk of complications.
Don’t be reluctant to make an appointment if you want professional guidance and extra suggestions on how to avoid athlete’s foot.
9. How to prevent Melasma?
Treating melasma:
Totally!
Three prescription medications are combined into one simple lotion for the most efficient treatment of melasma.Consistency is the key to preventing the progression or reappearance of melasma take your medication as directed and cover your skin from the sun even on overcast days.
It can take a few months before you notice the full improvements because melasma can be slow to respond to treatment.
However, results in terms of skin lightening could start to show in as little as a month.
1. Daily use of sunscreen:
Sunlight is one of the main causes of melasma, thus using sunscreen every day is essential to preventing it. Select a spectrum sunscreen that has an SPF of 30.
2. Outdoor headwear:
Widebrimmed hats assist shield the face’s delicate areas from the sun’s beams. When outside, seek out shade wherever possible.
3. Calming skin care:
Use soft products that don’t sting or burn because goods that irritate the skin make melasma worse.
Even the best skin care and precautions may not totally prevent melasma.
But in the vast majority of instances, measures taken to avoid it or treat it are effective in removing those bother spots.
With the right sun protection, melasma can be treated and prevented in many effective ways.
Wear sunscreen every day, whether it’s sunny or cloudy, because exposure to the sun causes this skin problem.
Choose spectrum sunscreens whenever possible & apply them at least every two hours.
Apply sunscreen more often if you’re going swimming or doing something else that makes you sweat a lot.
The most important thing to wear is sunscreen, but you may also shield yourself from the sun’s rays by wearing layered clothing, a wide-brimmed hat, and a baseball cap.
Put on some sunglasses to protect the delicate skin around your eyes, but make sure the style is appropriate.
Avert metal sunglasses.
If your melasma has cleared up, your physician might suggest maintenance therapy to stop it from coming again
No matter whatever course of treatment is appropriate for you, prevention is essential. When you’re outside, always wear a widebrimmed hat and sunscreen.
10. How to prevent Skin cancer?
Skin cancer specifically is the abnormal growing of skin cells and is typically brought on by excessive sun exposure and damaging ultraviolet (UV) rays.
Although the majority of instances involve exposed skin, fully covered body parts like your hands or the genital region can also be impacted.
Skin cancer can affect both dark and light pigmentations.
What can we do to prevent skin cancer?
We’ve advise the following five methods to prevent skin cancer:
Even in the winter and on cloudy days, stay out of the sun between the hours of 10 a.m. and 4 p.m., which are the peak hours of sun strength in North America.
Wear sunscreen all year long, preferably with an SPF of 30 or higher.
If you’re swimming or perspiring, reapply sunblock every two hours or more frequently.
Wear clothing that has a UV protection factor (UPF) of 50+ to protect yourself from the sun’s rays, which blocks 98 percent of them.
To shield your skin from damaging UV rays, wear hats with wide brims and sunprotective clothing that covers your arms and legs. Not all UV rays, which cause skin cancer, are blocked by sunscreen. Skip the tanning bed.
UV lamps used in tanning beds can harm your skin and possibly cause cancer.Examine your own skin. Discuss any changes you notice with your healthcare team.
The best way to prevent skin cancer is to use sun protection measures and stay out of the UV light’s path.
Preventive measures include limiting time spent in the sun (especially when the sun is at its strongest), avoiding tanning beds, frequently using sunscreen, and donning protective clothes and eyewear.
An essential component of living a healthy lifestyle is taking preventive measures against skin cancer.
One in five Americans may acquire skin cancer over their lifetime, making it the most prevalent type of cancer in the country.
Squamous cell carcinoma and basal cell carcinoma, the two most prevalent types of skin cancer, are generally curable if discovered early.
The majority of skin cancer fatalities are caused by melanoma, although this cancer can also be successfully treated if found early enough, before it spreads to the lymph nodes.
What do i do to reduce the risk of skin cancer?
The majority of skin malignancies are caused by excessive exposure to ultraviolet (UV) rays. UV rays are emitted by the sun, tanning beds, and sunlamps.
UV radiation can cause skin cell damage.To reduce your chances of developing skin cancer, protect your skin from UV radiation from the sun and avoid artificial forms of UV exposure such as tanning beds and sunlamps.
1. Practice sun safety:

UV ray protection is essential all year, not just in the summer. UV rays can reach you even on cloudy or cool days because they reflect off surfaces such as water, cement, sand, and snow.
UV rays are strongest in the continental United States from 10 a.m. to 4 p.m. during daylight saving time (9 a.m. to 3 p.m. standard).
2. Avoid indoor tanning:

Indoor tanning (darkening the skin with a tanning bed, booth, sunbed) exposes users to high quantities of UV radiation. Too much UV light exposure can lead to skin cancer, cataracts, and eye cancer over time.
A tan is not an indication of good health. When UV rays penetrate the skin’s inner layer, it produces more melanin
Melanin is the pigment responsible for skin colour.
It progresses to the skin’s outer layers and appears as a tan. Any change in skin tone following UV exposure (whether a burn) indicates harm rather than health.
All conditions that irritate, clog, or damage your skin, as well as skin cancer, are considered skin diseases.
You could be born with a skin condition or develop one.
Many skin diseases result in itching, dry skin, or rashes.
Medications, proper skin care, and lifestyle changes can often help you manage these symptoms.
Treatment, on the other hand, can reduce symptoms and even keep them at bay for months at a time.
Many skin conditions never completely disappear.
Also, keep an eye out for any changes in your skin, such as new or inhaling spots or changes in moles. Most skin cancers are curable if detected and treated early.